Cael's PK4 class made cards for Ryleigh, each one hand decorated with love from each of his 19 classmates!
Thank you Cael for thinking of your baby sister and asking your class to do such a wonderful deed.
Love,
mommy
Saturday, March 31, 2012
Flowers for Ryleigh
A big cheery thank you to the UK Walker's!
The flowers are lovely and will be a forever part of Ryleigh's blog!
Love,
the US Walker's
[Non] Expectations
Coming to Terms
What I have learned through this ordeal of coming to terms
with a child who will be born in need of extra special care and love, is that
it is a process. I cannot even begin to describe the agony, pain, and terror we
have felt the last two weeks. I have cried, grieved, mourned, smiled, laughed,
and most of all dreamed. My husband and
I have accepted that she will be in need of open-heart surgery when she is born,
and really try to stay away from the thought that we will only have a few minutes
with her upon birth to enjoy seeing her, smelling her, hearing her, kissing her,
and holding her – before she is wheeled to the NICU. I guess as I get closer to
delivery this reality will need to be accepted, but right now we feel it is a
one-step-at-a-time process, we are trying not to overwhelm ourselves, which is
really, really easy to do.
Find support
Other parents of TA kids and TA kids themselves have provided
us with tremendous support we can’t thank them enough for their encouragement
and for keeping it all real. We have joined several really great support groups
that have not only provided support, but reality – it has prepared us for the
long, hard journey we are about to face – but they inspire us to know her life
and our lives will be great:
Truncus Arteriosus Kids: https://www.facebook.com/#!/groups/74129260045/
Broken Hearts: https://www.facebook.com/#!/BrokenHeartsFL
Mended Little Hearts: https://www.facebook.com/#!/pages/Mended-Little-Hearts-National-Organization/377812750472
Our Truncus Arteriosus Kids: http://groups.yahoo.com/group/ourtruncusarteriosuskids/
Prepare
I have officially set Cael’s bedroom up to be a one stop
shop and have stocked it full of all the fun stuff he loves (he has enjoyed two
rooms before the news of a new addition). No more separate toy room for you!
Next we will begin to take all of the baby items we have received and purchased,
and begin the process of setting up Ryleigh’s room. When I think about seeing
her room set up, but empty I mourn, I can’t explain it, but it makes me sad. I
need to feel these emotions as with each tear that I cry, I am becoming
stronger.
Expect Disappointment,
but Find Hope
I need to say that I admire my husband, he is an amazing man
and I really can’t imagine going through this process with anyone else. I have
seen him reduced to tears, but yet still so strong. We are becoming stronger together
and the advice we have received is this has to happen to get through this
ordeal. We have had major upsets and disappointments this last week, and I can only
share that family has been one of the biggest disappointments and some of the
best supporters. At this point, we are moving on and letting go as our focus
needs to be on what is going to directly affect our lives and our son’s life.
It is about us and it has to be that way. I am not surprised how ugly people can
be, only surprised that the time they chose to display it, is a time of despair
and turmoil, kicking us while we are down is inexcusable. Several other TA moms
have shared that family hurt them the most because as we are hurting, we expect
so much more out of our support system.
We expect them to be there and not be selfish, but the reality is we can’t
change people and it is better to cut the negative people out than to try and make
them supportive. We have also found tremendous support in other family members and
friends when they know there is a gap in our support system, for that we can’t
thank you enough and you know who you all are!
A loved one recently told me that my husband, myself, Ryleigh,
and Cael are not losing anything, the loss will be felt on the end of those
that chose to alienate themselves. I agree. Last Thursday (3/29/12), we experienced
an upsetting situation that flared my heart condition and sent my own heart
into a type of cardiac arrest, along with the inability to breathe, which brought
on a full panic attack, my blood sugar dropped very low, which has never been
an issue with me. My husband called rescue and I was treated, I am happy to
report Ryleigh and mommy are now doing ok, but need to take it slow and stress
free for a long while. I feel bad that Cael had to go through that and see that
as he cried he said I thought you were dying, as a mom I never want him to see
that! I am so enamored with my husband’s
ability to remain calm even though it was an unnatural position to be in. Amazing man indeed. He saved my life and our
child’s life because he made the right decisions.
Other parents have stated don’t feel guilty for what you
cannot control, only focus on what you can control. Great advice and we are going
to take it!
Look to the Future
We have several appointments coming up and will share what
is going on as we know it. At this time we are putting on our big parents pants
and preparing for the arrival of our daughter in about 16 ½ weeks now. I just know the time will fly by.
As we look into the future, I am pleased to announce I am
now a doctor, yahoo I finished my degree, just in time! I would NOT have been
able to do this without the support of my crew: Craig, Cael, and Ryleigh!
Here’s to opening new doors and looking toward the rainbow.
Thursday, March 29, 2012
Mommy has one too...
It is not common to share heart defects through family lines, but I too have one but it is not related to or have any causal effect on what Ryleigh has, meaning one did not cause the other, we are just two peas in the pod sharing a commonality.
AV Heart Block
Atrioventricular (AV) block occurs when atrial depolarizations fail to reach the ventricles or when atrial depolarization is conducted with a delay. Three degrees of AV block are recognized.
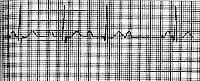
First-degree AV block consists of prolongation of the PR interval on the electrocardiogram (ECG) (> 200 msec in adults and > 160 msec in young children). The upper limit of the reference range for the PR interval is age-dependent in children. All atrial impulses reach the ventricles in first-degree AV block; however, conduction is delayed within the AV node (see the image below).
First-degree atrioventricular block. PR interval is constant and is 280 msec.
Second-degree AV block is characterized by atrial impulses (generally occurring at a regular rate) that fail to conduct to the ventricles in 1 of the following 4 ways.
The first form of second-degree AV block is Mobitz I second-degree AV block (Wenckebach block), which consists of progressive prolongation of the PR interval with the subsequent occurrence of a single nonconducted P wave that results in a pause. The pause is shorter than the sum of any 2 consecutive conducted beats (R-R interval).
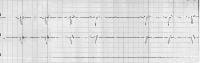
An episode of Mobitz I AV block usually consists of 3-5 beats, with a ratio of nonconducted to conducted beats of 4:3, 3:2, and so forth (see the image below). The block is generally in the AV node but can occasionally occur in the His-Purkinje system and is termed intrahisian or infrahisian Wenckebach (depending if the block occurs within or below the His-Purkinje system).
Second-degree atrioventricular block, Mobitz type I (Wenckebach). Note the prolongation of the PR interval preceding the dropped beat and the shortened PR interval following the dropped beat.
The second form is Mobitz II second-degree AV block, which is characterized by a constant PR interval followed by sudden failure of a P wave to be conducted to the ventricles, so that either an occasional dropped P wave or a regular conduction pattern of 2:1 (2 conducted and 1 blocked), 3:1 (3 conducted and 1 blocked), and so on is observed (see the image below).
Second-degree atrioventricular block, Mobitz type II. A constant PR interval in conducted beats is present. Intraventricular conduction delay also is present.
The third form is high-grade AV block, which consists of multiple P waves in a row that should conduct, but do not. The conduction ratio can be 3:1 or higher, and the PR interval of conducted beats is constant. This is a distinct form of complete AV block, in that the P waves that conduct to the QRS complexes occur at fixed intervals. For complete AV block, no relationship exists between the P waves and QRS complexes.
The fourth form is 2:1 AV block. This could be either Mobitz I or Mobitz II, but distinguishing one variety from the other is nearly impossible.
Third-degree AV block is diagnosed when no supraventricular impulses are conducted to the ventricles. P waves on the rhythm strip reflect a sinus node rhythm independent from QRS wave complexes. The QRS complexes represent an escape rhythm, either junctional or ventricular. The escape rhythm originating from the junctional or high septal region is characterized by narrow QRS complexes at a rate of 40-50 beats/min, whereas escape rhythm from low ventricular sites is characterized by broad QRS complexes at a rate of 30-40 beats/min.
No relationship exists between the rhythm of P waves and the rhythm of QRS complexes in third-degree AV block. The frequency of P waves (atrial rate) is higher than the frequency of QRS complexes (ventricular rate) (see the image below).
Third-degree atrioventricular block (complete heart block). The atrial rate is faster than the ventricular rate, and no association exists between the atrial and ventricular activity.
AV dissociation is a rhythm identified by atrial and ventricular activation occurring from different pacemakers. AV dissociation does not indicate the presence of AV block and is distinctly different. Ventricular activation may be from either junctional pacemakers or infranodal.
AV dissociation can occur in the presence of intact AV conduction, especially when rates of the pacemaker, either junctional or ventricular, exceed the atrial rate. Third-degree AV block can occur with AV dissociation. However, in AV dissociation without AV block, the ventricular rate can exceed the atrial rate and conduction can occasionally occur dependent on the timing between the P wave and the QRS complex.
AV block may also occur in patients with atrial fibrillation (see the Atrial Fibrillation Center). Regular R-R intervals are possible in the presence of AV block (generally at slow regular rates).
Tuesday, March 27, 2012
Letter to Ryleigh 3/27/12
My dear sweet Ryleigh,
I dedicate this blog to you so that we can share our journey with close friends and family. Also to see how far you come and to share the ups and downs with other Truncus families. One day you will be old enough to read it and see the love that was there from the moment you became a member of our family.
I wanted to write you a note today to let you know that my heart is full of love for you. In looking back at the moment your daddy and I decided we would try to have you, was one of the happiest times I can remember. The moment I found out you had gone from a twinkle in my eye to a conceived baby, I began to build hopes and dreams. We are 22 weeks along and in 17 weeks you will be born. I can’t express in words how excited and overjoyed I am to know that soon I will hold you in my arms. I know that day will be bittersweet because I know they are going to take you from me and your daddy to make you better.
I cannot describe at this moment how I'm going to feel when it is time for you to go, but know no matter where you are, mommy and daddy will always be with you. I look forward to the day when we get to see you smile, laugh, and play with your big brother Cael.
When I found out that we were having a little girl I was so elated. You have no idea how much I wanted you. I had so many hopes and dreams for you before we knew about your condition. And it's not that I don't now, knowing your condition, but I realize those hopes and dreams have changed. My hope is that you will live a long and happy life filled with everything you want to do. My dream is that one day you will meet a man as wonderful as your daddy that you will fall in love with and have little ones that capture your heart as you and Cael have done for me. You, Cael and your daddy are my life, my reason for breathing – when you are born I ask that you be strong and come home to me, to us.
I never want you to think that this condition will ever be a burden on our family because what you have given us is the true meaning of unconditional love. Now that I have felt you, heard you, and seen you through technology – there is no way I can lose you. I need you Ryleigh. We will love you like a perfect child even though your heart and my heart are broken. Your normal will become our new normal, and we will make the best of every moment. You have given me purpose like nothing ever before.
I was driving your big brother to school today and he was humming a sweet song. I asked him what the song was from and he said he was singing it for you. Did you hear him? He sings to you all the time, and he tells you how much he loves you each and every day. You two are going to be best friends! He is sweet and caring and wants to share in this journey, I can’t wait for you two to meet.
I'm going to go now, but I can feel you with each of your gentle kicks, which reassures me that you are with me and we are together not matter what. I will write more soon.
Love you always,
mommy, daddy, and Cael
Monday, March 26, 2012
What the heck is Truncus Arteriosus?
Ryleigh has a condition called...
Info courtesy of: http://community.e-baptisthealth.com/health-info/content/ped/eng/cardiac/truncus.html

Click Image to Enlarge

Click Image to Enlarge
Info courtesy of: http://community.e-baptisthealth.com/health-info/content/ped/eng/cardiac/truncus.html
Truncus Arteriosus
What is truncus arteriosus?

Click Image to Enlarge
Truncus arteriosus is a congenital (present at birth) defect that occurs due to abnormal development of the fetal heart during the first 8 weeks of pregnancy. The heart begins as a hollow tube, and the chambers, valves, and great arteries develop throughout the first 8 weeks of pregnancy. The aorta and pulmonary artery start as a single blood vessel, which eventually divides and becomes two separate arteries. Truncus arteriosus occurs when the single great vessel fails to separate completely, leaving a connection between the aorta and pulmonary artery.
Truncus arteriosis is a complex defect where there is a single (normally there are two separate arteries) vessel arising from the heart that forms the aorta and pulmonary artery. Another congenital heart defect that occurs with truncus arteriosus is a ventricular septal defect (ventricular septum, or dividing wall between the two lower chambers of the heart known as the right and left ventricles).
Normally, there are two separate arteries (the aorta and the pulmonary artery. Oxygen-poor (blue) blood returns to the right atrium from the body, travels to the right ventricle, then is pumped through the pulmonary artery into the lungs where it receives oxygen. Oxygen-rich (red) blood returns to the left atrium from the lungs, passes into the left ventricle, and then is pumped through the aorta out to the body.

Click Image to Enlarge
In truncus arteriosus, oxygen-poor (blue) and oxygen-rich (red) blood mix back and forth through the ventricular septal defect. This mixed blood then flows through the common truncal vessel. Some of it will flow through the branch that becomes the pulmonary artery and on to the lungs, and some of the mixed blood will go into the aortic branch and continue to the body. The mixed blood that goes to the body does not have as much oxygen as normal, and will cause varying degrees of cyanosis (blue color of the skin, lips, and nailbeds).
Truncus arteriosus occurs in less than one out of every 10,000 live births. It makes up 1 percent of all cases of congenital heart disease.
What causes truncus arteriosus?
Some congenital heart defects may have a genetic link, either occurring due to a defect in a gene, a chromosome abnormality, or environmental exposure, causing heart problems to occur more often in certain families. Other times this heart defect occurs sporadically (by chance), with no clear reason for its development.
Why is truncus arteriosus a concern?
The blood that passes through the common truncal vessel has a lower oxygen content than normal. Oxygen-poor (blue) blood from the right ventricle and oxygen-rich (red) blood from the left ventricle mix together before entering the common vessel. Some of this mixed blood will go into the aorta and on to the body, producing cyanosis (blue color of the skin, lips, and nailbeds).
The pulmonary artery section of the common vessel gets more blood flow than the aorta does, because the pressure is lower in the lungs than the body and it is easier for blood to travel in that direction. If not repaired, the blood vessels in the lungs become damaged by the extra blood flow. As the pressure in the blood vessels in the lungs becomes higher, less blood goes to the lungs and more goes to the body. Cyanosis becomes worse as blood with lower amounts of oxygen travels to the body.
What are the symptoms of truncus arteriosus?
The following are the most common symptoms of truncus arteriosus. However, each child may experience symptoms differently. Symptoms may include:
- cyanosis
- fatigue
- sweating
- pale skin
- cool skin
- rapid breathing
- heavy breathing
- rapid heart rate
- congested breathing
- disinterest in feeding, or tiring while feeding
- poor weight gain
The symptoms of truncus arteriosus may resemble other medical conditions or heart problems. Always consult your child's physician for a diagnosis.
How is truncus arteriosus diagnosed?
Your child's physician may have heard a heart murmur during a physical examination, and referred your child to a pediatric cardiologist for a diagnosis. A heart murmur is simply a noise caused by the turbulence of blood flowing through the heart defects. Symptoms your child exhibits will also help with the diagnosis.
A pediatric cardiologist specializes in the diagnosis and medical management of congenital heart defects, as well as heart problems that may develop later in childhood. The cardiologist will perform a physical examination, listening to the heart and lungs, and make other observations that help in the diagnosis. The location within the chest that the murmur is heard best, as well as the loudness and quality of the murmur (harsh, blowing, etc.) will give the cardiologist an initial idea of which heart problem your child may have. However, other tests are needed to help with the diagnosis, and may include the following:
- chest x-ray - a diagnostic test which uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film.
- electrocardiogram (ECG or EKG) - a test that records the electrical activity of the heart, shows abnormal rhythms (arrhythmias or dysrhythmias), and detects heart muscle stress.
- echocardiogram (echo) - a procedure that evaluates the structure and function of the heart by using sound waves recorded on an electronic sensor that produce a moving picture of the heart and heart valves.
- cardiac catheterization - a cardiac catheterization is an invasive procedure that gives very detailed information about the structures inside the heart. Under sedation, a small, thin, flexible tube (catheter) is inserted into a blood vessel in the groin, and guided to the inside of the heart. Blood pressure and oxygen measurements are taken in the four chambers of the heart, as well as the pulmonary artery and aorta. Contrast dye is also injected to more clearly visualize the structures inside the heart.
Treatment for truncus arteriosus:
Specific treatment for truncus arteriosus will be determined by your child's physician based on:
- your child's age, overall health, and medical history
- extent of the condition
- your child's tolerance for specific medications, procedures, or therapies
- expectations for the course of the condition
- your opinion or preference
Truncus arteriosus must be treated by surgical repair of the defects. However, medical support may be necessary until the best time for the operation to take place. Treatment may include:
- medical management
Many children will eventually need to take medications to help the heart and lungs work better. Medication that may be prescribed includes the following:- digoxin - a medication that helps strengthen the heart muscle, enabling it to pump more efficiently.
- diuretics - the body's water balance can be affected when the heart is not working as well as it could. These medications help the kidneys remove excess fluid from the body.
- ACE (angiotensin-converting enzyme) inhibitors - dilates the blood vessels, making it easier for the heart to pump blood forward into the body.
- adequate nutrition
Infants may become tired when feeding, and may not be able to eat enough calories to gain weight. Options that can be used to ensure your baby will have adequate nutrition include:- high-calorie formula or breast milk
Special nutritional supplements may be added to formula or pumped breast milk that increase the number of calories in each ounce, thereby allowing your baby to drink less and still consume enough calories to grow. - supplemental tube feedings
Feedings given through a small, flexible tube that passes through the nose, down the esophagus, and into the stomach, can either supplement or take the place of bottle feedings. Infants who can drink part of their bottle, but not all, may be fed the remainder through the feeding tube. Infants who are too tired to bottle feed may receive their formula or breast milk through the feeding tube alone.
- high-calorie formula or breast milk
- surgical repair
Surgery is usually performed after the infant is 2 weeks old, but before the blood vessels in the lungs are overwhelmed by extra blood flow and become diseased.
The operation is performed under general anesthesia, and involves the following:- The pulmonary arteries are detached from the common artery (truncus arteriosus) and connected to the right ventricle using a homograft (a section of pulmonary artery with its valves intact from a tissue donor).
- The ventricular septal defect is closed with a patch.
Postoperative care for your child:
Children will spend time in the intensive care unit (ICU) after a truncus repair.
While your child is in the ICU, special equipment will be used to help him/her recover, and may include the following:
- ventilator - a machine that helps your child breathe while he/she is under anesthesia during the operation. A small, plastic tube is guided into the windpipe and attached to the ventilator, which breathes for your child while he/she is too sleepy to breathe effectively on his/her own. After a truncus repair, children will benefit from remaining on the ventilator overnight or even longer so they can rest.
- intravenous (IV) catheters - small, plastic tubes inserted through the skin into blood vessels to provide IV fluids and important medicines that help your child recover from the operation.
- arterial line - a specialized IV placed in the wrist or other area of the body where a pulse can be felt, that measures blood pressure continuously during surgery and while your child is in the ICU.
- nasogastric (NG) tube - a small, flexible tube that keeps the stomach drained of acid and gas bubbles that may build up during surgery.
- urinary catheter - a small, flexible tube that allows urine to drain out of the bladder and accurately measures how much urine the body makes, which helps determine how well the heart is functioning. After surgery, the heart will be a little weaker than it was before, and, therefore, the body may start to hold onto fluid, causing swelling and puffiness. Diuretics may be given to help the kidneys to remove excess fluid from the body.
- chest tube - a drainage tube may be inserted to keep the chest free of blood that would otherwise accumulate after the incision is closed. Bleeding may occur for several hours, or even a few days after surgery.
- heart monitor - a machine that constantly displays a picture of your child's heart rhythm, and monitors heart rate, arterial blood pressure, and other values.
Your child may need other equipment not mentioned here to provide support while in the ICU, or afterwards. The hospital staff will explain all of the necessary equipment to you.
Your child will be kept as comfortable as possible with several different medications; some which relieve pain, and some which relieve anxiety. The staff will also be asking for your input as to how best to soothe and comfort your child.
After discharged from the ICU, your child will recuperate on another hospital unit for a few days before going home. You will learn how to care for your child at home before your child is discharged. Your child may need to take medications for a while at home, and these will be explained to you. The staff will give you instructions regarding medications, activity limitations, and follow-up appointments before your child is discharged.
Caring for your child at home following truncus arteriosus repair:
Pain medications, such as acetaminophen or ibuprofen, may be recommended to keep your child comfortable at home. Your child's physician will discuss pain control before your child is discharged from the hospital.
Often, infants who fed poorly prior to surgery have more energy after the recuperation period, and begin to eat better and gain weight faster. However, high-calorie formulas may be needed for several weeks or months after surgery to help your child catch up growth-wise. Tube feedings may also be helpful until your child is able to feed better.
After surgery, older children usually have a fair tolerance for activity. Your child may become tired easily, and sleep more right after surgery, but, within a few weeks, your child should be fully recovered.
You may receive additional instructions from your child's physicians and the hospital staff.
Long-term outlook after truncus arteriosus surgical repair:
Many children who have had truncus arteriosus surgical repair can live healthy lives. Activity levels, appetite, and growth will eventually return to normal in most children.
Future intervention may be necessary if the pulmonary artery branches were small and do not grow well after surgery. The homograft connecting the right ventricle to the pulmonary artery may also need to be replaced in the future as your child grows.
Your child's cardiologist may recommend that antibiotics be given to prevent bacterial endocarditis after discharge from the hospital.
Regular follow-up care at a center offering pediatric or adult congenital cardiac care should continue throughout the individual’s lifespan.
Consult your child's physician regarding the specific outlook for your child.
5 days with the news...
My name is Lee Ann and my husband’s name is Craig, we have a perfect little boy Cael who is 5. We are currently pregnant with our 2nd buddle of joy. I am 5 ½ months along. I was referred out to a specialist in my town because of my age (38), which they say is old now for kids. We went at 18 weeks and had our anatomy scan and gender identification. I wanted so desperately a girl, so when the u/s tech said do you want to know we both said YES! She said it is a girl! Tears streamed down my face, it was a happy moment for me! Then as quickly as the moment came the bad news poured in. The doctor came in and described to us that she had a brain malformation also common with Dandy Walker Syndrome. He said it was a concern as her cisterna magna was 8mm and should have been only 6.9. So he said come back in 4 week and we will recheck when we do your fetal echo. It was the longest 4 weeks of my life, I cried for days!!! I was asked to take the Quad Screen, which I did and passed with no issues, all came back negative. They told us the baby did not have a cleft lip, or any other u/s malformations at that time (nasal bone was present and 2 bends in the pinkie) and we should just watch this brain issue – as at 18 weeks it is not all there.
The 4 weeks had passed and we were confident walking in that we had done our research and this was of medical insignificance because it was an isolated finding. They rescanned the brain and the doctor said we can down grade this to a cyst, which is a variant of DW – all parts of the brain are present and appear to be great. Whew! We were so happy. The joy was short lived, that lasted for about 2 minutes until they then told us the heart had an issue. The doctor asked if I could stick around to see another doctor, I was not understanding him at first, tears streaming down my face, my brain was screaming on the inside, all I saw was anger – how could he keep doing this to us? I said what is wrong now? That is when the news hit me like a chain wrapped around my neck pulling me to a dark place. He said your baby has a condition known as truncus arteriosus, I could not even say it. He asked the u/s tech to write it down for us. I said I could not handle anymore I needed to go home – I was sick with agony. They called us that afternoon to see if we could see a pediatric cardiologist the next day (Wednesday, March 21, 2012). We went the next day and she explained to us what this was, showing us a normal heart and our little Ryleigh’s heart. She then explained what needed to be done, and what we should expect. She said we will have our best University of Florida cardiac pediatricians performing the surgery along with a highley skilled peds team at Wolfson's Childrens Hospital on the case. It has been 5 days now that we were told this news. My mind has not stoppped thinking. I feel guilt, shame, blame, and all of the above. I am working through the emotions and with the support of my wonderful husband we will make it and Ryleigh will too! Afterall she has too, she is my little girl.
Subscribe to:
Comments (Atom)

.JPG)